This is considered the standard for state-of-the-art imaging and is ideal for abdomen and chest MRIs.
Same as the 1.5T MRI, but with an open design. Open MRI and Wide-Open MRI are useful for patients who tend to be claustrophobic or who are too large to fit into a closed MRI. Such patients no longer have to sacrifice image quality, or rely on sedatives, thanks to the combination of high strength magnets with more open designs. Certain open machines have tables that lower to wheelchair height, for greater patient comfort.
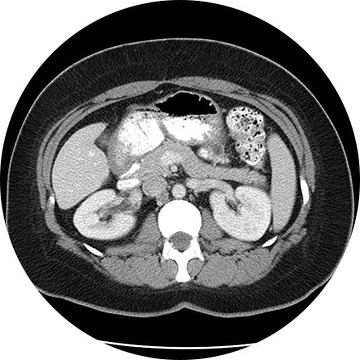
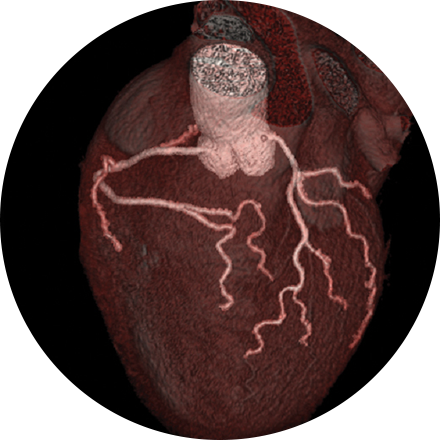
The high-resolution medical images in 3D show a remarkable real-life appearance of your internal organs. The technology is far advanced over traditional CT imaging and provides excellent diagnostic information. Whole body scanning, coronary artery calcium scoring, virtual colonoscopy, lung screening, heart scanning—these are the advanced 3D imaging procedures available to patients at our facilities.
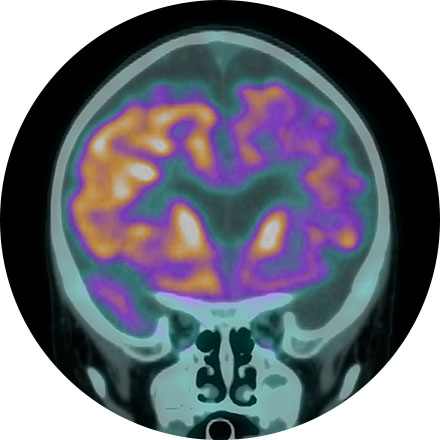
Description for Alzheimer’s Evaluation.
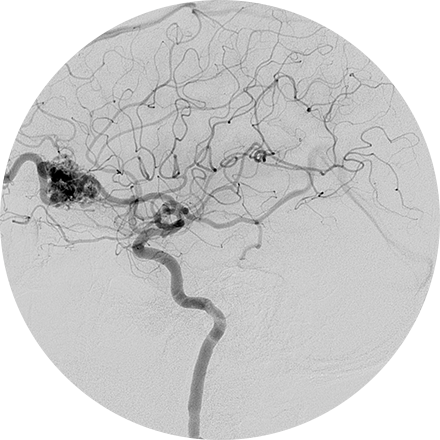
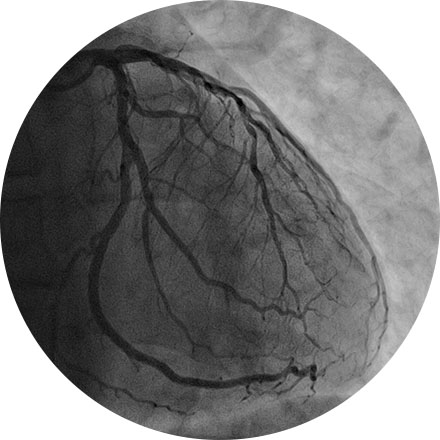
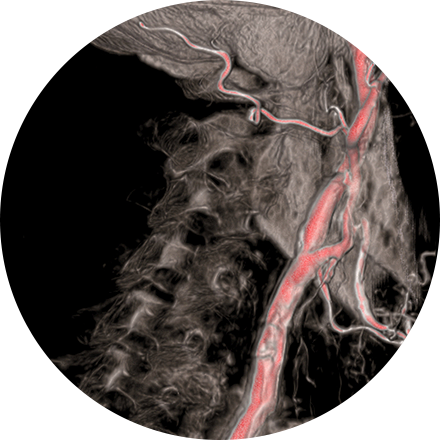
An angiogram is an X-ray exam of the arteries and veins to diagnose blockages and other blood vessel problems. It can reveal the integrity of the cardiovascular system in specific areas throughout the body. Combined with the use of intravenous contrast medium injected via a catheter, an angiogram identifies areas of blockage or damaged vessels within the circulatory system. CT and MRI may also be used to gain additional images of the arteries.
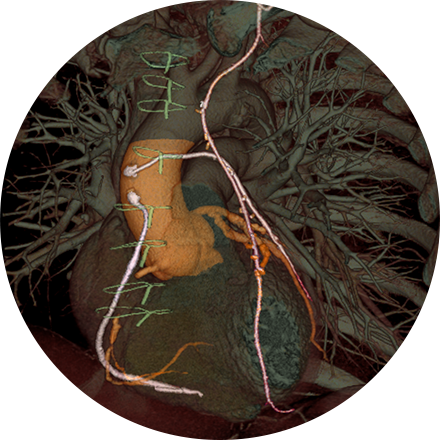
Often the first choice procedure after a heart attack, a catheter is threaded into the coronary arteries where a stent or balloon is also guided to create more space for blood to flow. Imaging and contrast agents are used to guide placement of the materials and to monitor blood flow.
An arthrogram is an X-ray exam of a joint, using a contrast agent and fluoroscopy (a live motion X-Ray). It is used to diagnose the cause of pain or restricted motion of a joint as well as injury to the components of the joint including, the tendons, soft tissues, ligaments, labrum, cartilage and bones. Often this procedure is used to image the shoulder and hip joints, and it is also used when investigating the knees, elbows, ankles and wrists. CT and MRI may also be used to gain additional images of the joint.
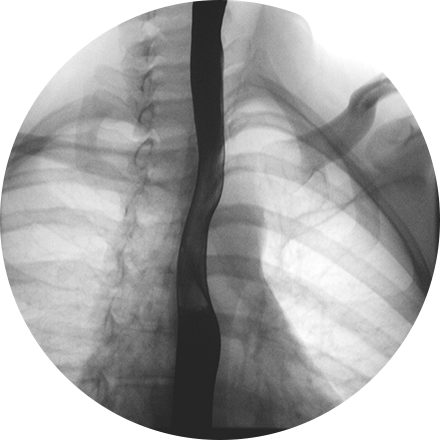
When a patient has chronic abdominal pain, bowel changes, reflux, unexplained vomiting, constipation, diarrhea, blood in the stool or cancer or tumors, a physician may request examination of the upper or lower gastrointestinal tract. The upper GI tract is the esophagus, stomach and first part of the small intestine. The lower GI tract is the large intestine (colon). Barium is an orally-ingested contrast used with fluoroscopy to image these organs in motion. This helps the physician gain an accurate understanding of the function and anatomy of those organs in the patient’s body.
These types of procedures treat blockages or narrowing of the bile ducts, sometimes caused by gallstones and leading to jaundice and severe inflammation or infection of the gall bladder. An interventional radiologist can perform a minimally invasive procedure (with imaging guidance and a contrast agent) that is appropriate for the pathology. The range includes draining of the bile, removal of gallstones, stent placement and decompression (of an inflamed gall bladder).
Biopsies (removal of tissue for investigation) may be performed with the guidance of CT, MR, ultrasound or X-ray images. If a lesion is discovered, a bone biopsy is performed through the skin to determine whether cancer or infection is present.
We provide diagnostic, palliative and therapeutic procedures to address bone cancer. DEXA scans help physicians evaluate the health of bone, and monitor its degeneration or stability over time. An image-guided biopsy, usually using fluoroscopy and contrast, may be used to help diagnose lesions and cell samples from bone. Vascular interventions can direct cancer-fighting drugs to specific locations in the body, without affecting other areas. Vertebroplasty can help alleviate pain symptoms from compressed or collapsed vertebrae.
Your provider may request a breast biopsy if a lump or abnormality is found during screening. A biopsy is a very accurate, minimally invasive method of locating and removing tissue for further investigation. Image-guided biopsy allows patients to avoid hospitalization and general anesthesia (previously necessary with traditional surgical biopsy). It is a valuable method of getting a fast, accurate, conclusive diagnosis—without unnecessary time, pain or expense to the patient.
Depending on your medical needs, we provide different diagnostic biopsy procedures:
Stereotactic biopsy uses mammography to precisely guide clinicians to a lump or abnormality that can’t be felt or seen on ultrasound. Clinicians see a 3D picture of the lump’s exact location.
MRI-guided biopsy uses MRI to guide the radiologist to the exact location of the lump. MRI biopsy is usually used when the lump can be seen on breast MRI, but cannot be readily seen on mammogram or ultrasound.
What happens during a biopsy procedure?
While the biopsy is performed, you will either remain seated in a comfortable, upright position or you will lie face down on a special table that allows your breast to be placed in an opening. The radiologist performs a core needle or vacuum-assisted biopsy (see below) while your breast is somewhat compressed in the mammographic biopsy system. You can return home in 30 minutes.
Vacuum-assisted biopsy devices are used for stereotactic and MRI guided biopsy and selected="selected" ultrasound guided biopsies. The device is a special probe that applies suction and allows retrieval of more tissue. Breast tissue is drawn into the sampling chamber of the probe with the vacuum and then cut. Several pieces of tissue are always obtained during biopsies, regardless of the type of needle used.
In a core needle biopsy, the radiologist locates the lump or abnormality that can be seen on a mammogram, sonogram or MRI. A hollow core needle is then placed inside the abnormality. The needle will then withdraw a small amount of tissue that will be sent to a lab for analysis. Prior to the procedure, you will be given some local anesthetic similar to the anesthetic used for dental procedures to numb the area. You may feel some pressure and mild discomfort but most patients do not feel pain. The doctor will insert the needle several times to get adequate tissue samples. After the procedure, you can resume normal activities immediately. You may experience some slight bruising but should not have a scar. It may take several days to one week to obtain results from the lab.
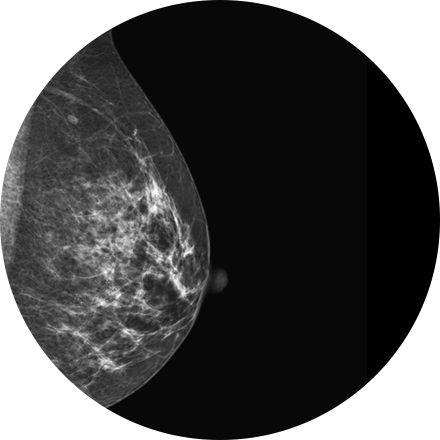
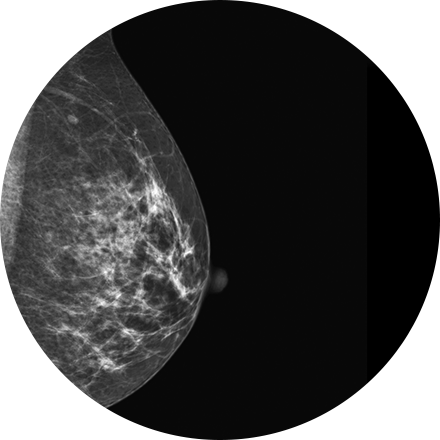
Breast cancer is the second most common cancer in women (after lung cancer), and early detection of breast cancer vastly increases survival rates. Scheduling a regular mammogram is one of the most important things you can do to ensure your well-being and take control of your health. We provide advanced screening and diagnostic procedures, such as Breast MRI and a range of biopsies. We offer a comprehensive breast imaging services.
Some women — because of their family history, a genetic tendency or certain other factors — should be screened with MRI in addition to mammograms. The number of women who fall into this category is small: less than 2 percent of all the women in the United States. Talk with your doctor about your history and whether you should have additional tests.
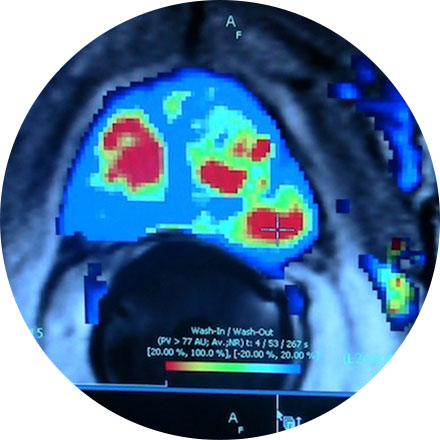
Breast MRI helps to detect small lesions sometimes missed by mammography — without using radiation or compressing the breasts. MRI uses powerful magnets and radio waves to take very clear pictures of soft tissues, so it can be extremely useful in breast imaging.
Ultrasound uses sound waves instead of X-rays to exam breast tissue. A transducer is passed over the breast. The transmitted sound waves are translated into a picture on a monitor. It does not cause discomfort and, because it does not use radiation, it carries very little risk.
Ultrasound is useful for women with dense breasts or for evaluating suspicious areas seen by mammography or felt during a breast exam. It can also find breast lesions that are close to the chest, where mammography is less useful. Breast ultrasound can distinguish between cysts, which are fluid-filled, versus other types of solid breast masses.
Cardiac MRI is used to obtain detailed images of the heart. It helps physicians evaluate heart structures, such as the cardiac chambers and valves, major vessels and the pericardium (a small structure that surrounds the heart). Disorders such as coronary artery disease, irreversible scarring after a heart attack, tumors, infections, and inflammation can all be diagnosed and monitored using MRI. Physicians also use MRI to plan future patient’s treatment.
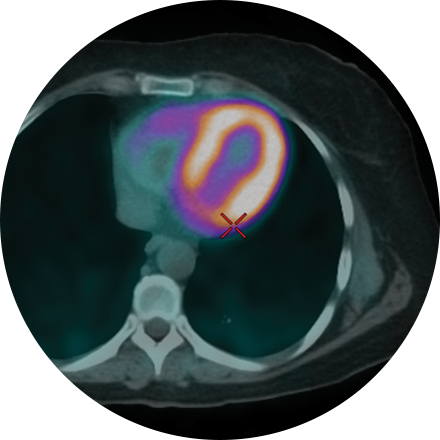
PET scans provide unique information on the metabolic functioning, rather than the structure, of the heart and other organs. Cardiac PET exams use tracer drugs to illuminate the area in question. A PET stress test can very accurately reveal complete or partial blockages to the arteries of the heart, enabling the patient to avoid an invasive catheterization in some cases.
This procedure allows doctors and nurses to easily access the venous system to repeatedly draw blood or to inject substances into the body. This procedure is useful when you need ongoing chemotherapy, antibiotic therapy, parenteral nutrition or kidney dialysis. In these procedures, the radiologist uses ultrasound to guide the placement of a thin catheter or other device into your chest, neck, or arm. Some common vein access procedures include:
Kidney dialysis access management – Central venous access is increasingly used in kidney dialysis.
Mediports (also called port-a-caths) – Devices are usually implanted in the upper chest to act as an I.V. into the bloodstream; they are used to deliver chemotherapy, medications, fluids, or to withdraw blood. PICCs (peripherally inserted central catheters) – Catheters inserted into the arm vein are threaded carefully to the superior vena cava, the large vein that connects to the heart.
PICCs are used for long-term intravenous antibiotics, chemotherapy, etc. and to prevent repeat needle sticks.
A chest X-ray is a very common medical procedure that can reveal the cause of chest pain, persistent cough or difficulty breathing. A very small dose of radiation is used to image the lungs, heart and other structures in the chest.
This exam is part of a sophisticated high-speed CT exam of the heart. During the scan, which takes just seconds, the equipment measures the amount of calcium present and calculates a score. The lower the score, the lower the potential risk of an adverse future cardiac injury. (Calcium often covers the atherosclerotic plaque that builds up inside arteries. This plaque and calcium can lead to narrowing of the inside of the arteries which could in turn lead to an increased risk of angina, and a heart attack.) This test can assess coronary heart disease, which is often asymptomatic and is the most common cause of death for patients in the United States.
Hormone replacement therapy, oral contraceptives and pregnancy are risk factors for DVT, the formation of a blood clot, known as a thrombus, in a deep leg vein. If DVT is untreated, it can break off and travel to the lungs, blocking the oxygen supply and triggering a heart attack. Your physician may order catheter-directed thrombolysis to break up the clot. This procedure threads a catheter through the veins to the clot, using imaging to guide the physician. A drug is then infused to that area, also pinpointed by radiology imaging. Angioplasty, stents, or vena cava filters may also be used.
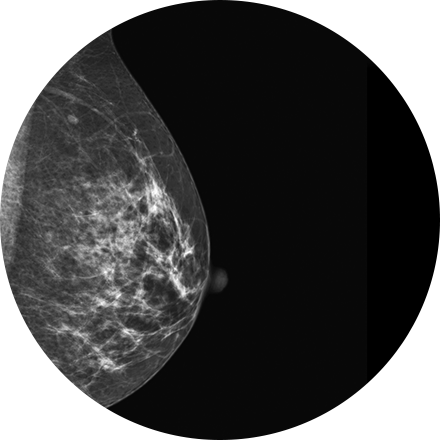
Mammography is a type of low-dose X-ray of the breast. It reveals masses and micro-calcifications within and around the breast that may indicate breast problems including, but not just limited to cancer.
Experts recommend a mammography screening of the breasts at regular intervals to increase the chance of early cancer detection and treatment. The American College of Radiology recommends women aged 40 and older should have a screening mammogram every year and should continue to do so for as long as they are in good health.
Discography is a procedure used to confirm that an abnormal disc is the culprit of pain. It is often used prior to a more invasive surgical procedure, to gather more information before that next step is taken. A contrast agent is introduced, and after the procedure a CT scan identifies leakage from the discs to identify any spinal disc herniation.
Embolization is used to stop unwanted bleeding, as with a wound or aneurysm (ruptured or unruptured). Medications or synthetic materials (embolic agents) are placed through a catheter into a blood vessel to prevent blood flow to the affected area.
This is an accurate and noninvasive imaging procedure used to assess and evaluate certain gastrointestinal problems, such as inflammatory bowel disease (including Crohn’s Disease), infectious enteritis, lymphoma or tuberculosis. It also can be used in patients with gastrointestinal bleeding to determine if a small bowel polyp is causing the bleeding. Enterography may be performed using MRI or CT.
The most common organs to be examined using fluoroscopy in children are the gastrointestinal tract (esophagus, stomach, small and large intestines) and the urinary tract (bladder, ureters, urethra). These studies involve contrast and, in some cases, a period of fasting before the exam.
Interventional procedures often provide invaluable assistance to your urologist or other physician for problems of the genitals and urinary tract. A few of the common procedures we perform include:
Nephrostomy – Placement of a tube into the kidney to allow urine to drain directly out of the body.
Kidney stone treatment – Manipulation and management of kidney stones with minimally invasive techniques.
Biliary procedures – Viewing and/or treating problems of the bile ducts, liver and gallbladder, including bile stones. These procedures include percutaneous cholangiogram (a contrast x-ray to find obstructions in the bile ducts), biliary stone removal (when they cannot be removed surgically) and biliary stent placement (for temporary relief from bile stone obstructions).
This scanner provides high image quality with no sacrifice to patient comfort.
Hysterosalpingography (HSG) in an outpatient procedure in which a special iodine-containing dye is injected through the cervix. It flows into the uterine cavity and through the fallopian tubes. If the tubes are not blocked, the dye will spill out of the tubes into the abdomen, indicating no obstruction is present. One or more X-Rays are taken during the procedure to provide permanent record of the condition of the fallopian tubes and uterine cavity. The actual progress of dye flowing through the tubes can be followed on a fluoroscopy monitor. Usually, HSG is performed within the first ten days of the start of a normal menstrual period.
Radiologists can diagnose and treat medical illness in children using small instruments such as catheters or tubes. Doctors guide small needles, catheters and other small medical equipment into the body through tiny incisions in the skin. The instruments are used to target and treat diseases, such as tumors and other abnormalities, at their source in the body.
In some cases, these treatments can solve problems faster and with smaller incisions than can other techniques, resulting in less pain and a shorter time to heal. In other cases, they can help treat medical problems that cannot be solved any other way.
The most common form of kidney cancer is renal cell carcinoma, which forms in the lining of the renal tubules that filter blood and produce urine. Often these small tumors are asymptomatic and only found on CT or MRI exams. Image-guided biopsy, usually using fluoroscopy and contrast, may be used to obtain and investigate tissue samples. Cryoablation is proving effective as a means of treating certain kidney tumors with a same-day procedure, instead of invasive surgery. Cryoablation uses extremely cold gas, an “ice ball,” directly on the tumor (via an image-guided probe) to destroy frozen tumor cells. Embolization may also be used to restrict large tumors that are invading other structures.
Image-guided biopsy, usually using fluoroscopy and contrast, may be used to obtain and investigate liver tissue samples for diagnosis. Surgery can be difficult for some liver tumors, if they are small or if they have grown into blood vessels. Interventional radiology can, in those cases, provide alternatives to surgery. Ablation and embolization can target the liver’s cancerous cells.
3D mammography (tomosynthesis) is an FDA-approved technology that complements conventional 2D mammography. While traditional mammography generates 2D images, 3D mammography creates multiple thin 3D image slices that allow each section of the breast tissue to be seen more clearly.
New imaging software used with our 3D mammogram units enables us to offer a lower-dose 3D exam. The software eliminates the need to obtain additional 2D images as part of the 3D exam, as previously required. This reduces the radiation dose, making it similar to that of a traditional 2D mammogram.
A 3D mammogram looks and feels like a regular mammogram. An x-ray arm scans over your breast taking multiple 3D images at various angles. Each scan takes about 4 seconds and the entire 3D mammogram lasts about 15-20 minutes.
When a lesion is found on the lung, a biopsy may be necessary to determine the exact nature of that lesion. Needle biopsies (or aspirations) remove cells from the lesion for further investigation. In a pleural biopsy, the pleural membrane, the layer of tissue that lines the pleural cavity is sampled. Interventional radiologists use CT, MRI, fluoroscopy and ultrasound to guide instruments to the exact location.
Smoking is the leading risk factor for lung cancer, and the lung is the most common site for primary cancer worldwide. In addition to highly accurate CT screening of the lungs for at-risk patients, we provide biopsy as a diagnostic tool. An image-guided biopsy, usually using fluoroscopy and contrast, may be used to investigate lesions and tissue samples from the lungs. We also provide ablation as a therapeutic intervention. Ablation is the insertion of needle electrodes directly into the site of a tumor in the lungs. The radio waves emitted by the probe create heat in the tissue, which kills cancerous cells in a small area around the probe.
A lung scan helps clinicians examine your lungs using a radionuclide and X-rays. A radionuclide is injected, and a camera can image how that liquid circulates in your bloodstream, specifically the supply to your lungs. You might also be asked to breathe a small amount of radionuclide mixed with oxygen through a face mask. The camera records where the air is going inside your lungs.
MRI-guided biopsy uses MRI to guide the radiologist to the exact location of the area of concern. MRI biopsy is usually used when the abnormality can be best seen on breast MRI, but not as well visualized on mammogram or ultrasound. Often lesions that are biopsied are done under the imaging modality that best demonstrates them.
Image-guided biopsy allows patients to avoid hospitalization and general anesthesia (previously necessary with traditional surgical biopsy). It is a valuable method of getting a fast, accurate, conclusive diagnosis—without unnecessary time, pain or expense to the patient.
Myelography is an exam in which contrast material is injected into your spinal column and then that contrast and spinal anatomy is imaged with CT technique. This allows the neuroradiologists to evaluate areas of nerve root impingement, canal narrowing, or disc protrusions. It is typically used when a patient is not a candidate for MRI.
NeuroQuant (NQ) is an artificial intelligence (AI) tool that calculates the volume of different substructures of the brain and compares those to a large normative age- and gender-matched database to determine whether the degree of brain volume loss is statistically significant for patient age. This can be used to improve the early detection of Alzheimer’s Disease (AD) or other neurodementia syndromes. NeuroQuant-MS is used to calculate the volume, number, and location of plaques in patients with multiple sclerosis. The software highlights new, enlarging, or shrinking plaques. This allows for accurate tracking of disease status over time. NQ can also be used to detect the location of a seizure focus in patients with epilepsy. It is also used in brain trauma patients or to assess brain development. Neuro-Quant has both MRI and CT applications. Other NeuroQuant-based AI tools in development include volumetric quantification and characterization of brain tumors.
A nuclear “stress test” takes images of your heart at rest and after your heart has been “stressed.” The two are compared to reveal if there is any damage to your heart muscle. This procedure helps evaluate coronary artery disease, acute chest pain, hibernating myocardium and cardiomyopathies. Initially, you will be injected with an isotope, and (30 minutes later) resting images will be acquired. The stress portion is next, which involves either a treadmill or injection of medications that mimic physiological stress. A second isotope is injected for this portion of the test. After your heart rate returns to normal and you eat, the technologist takes the final set of images of your heart.
Cardiac nuclear medicine studies help physicians diagnose the cause and exact location of chest pain and visualize blood flow patterns to the heart (myocardial perfusion scan), scan for heart attack damage, assess the heart post-surgery (bypass or re-vascularization), and see the heart-wall movement (in conjunction with an electrocardiogram, or ECG).
A nuclear “stress test” takes images of your heart at rest and after your heart has been “stressed.” The two are compared to reveal if there is any damage to your heart muscle. This procedure helps evaluate coronary artery disease, acute chest pain, hibernating myocardium and cardiomyopathies. Initially, you will be injected with an isotope, and (30 minutes later) resting images will be acquired. The stress portion is next, which involves either a treadmill or injection of medications that mimic physiological stress. A second isotope is injected for this portion of the test. After your heart rate returns to normal and you eat, the technologist takes the final set of images of your heart.
Open MRI and Wide-Open MRI are useful for patients who tend to be claustrophobic or who are too large to fit into a closed MRI machine. Such patients no longer have to sacrifice image quality, or rely on sedatives, thanks to the combination of high strength magnets with more open designs. Certain open machines have tables that lower to wheelchair height, for greater patient comfort.
Osteoporosis affects 10 million Americans and is responsible for 700,000 vertebral fractures each year. The disease is symptomless until a fracture occurs; fractures can cause stopped posture, compression of the lungs and stomach, chronic pain, and loss of independence. In addition to bone scans to reveal the health of bone structures, we provide non-surgical vertebroplasty for relief from spinal pain.
We provide a range of interventional procedures for the management of spinal pain. They include:
Vertebroplasty and kyphoplasty are procedures that treat spinal fractures or compressed / collapsed vertebrae, often performed by a neuroradiologist. Vertebroplasty is the injection of a cement-like material into the bone to make it more stable. In kyphoplasty, the doctor first creates space by inflating a balloon-like device in the bone. The space is then filled with the cement material.
Discography is a procedure used to confirm that an abnormal disc is the culprit of pain. It is often used prior to a more invasive surgical procedure, to gather more information before that next step is taken. A contrast agent is introduced, and after the procedure a CT scan identifies leakage from the discs to identify any spinal disc herniation.
Facet and SI joint injections are used to alleviate joint pain, such as with arthritis or injury, or to determine the exact cause of pain. Under X-ray guidance, a clinician injects anesthetic directly into the joint or anesthetizes the nerves to carry pain signals away from the joint.
Nerve root injections are used to help ease back and leg pain when a nerve is inflamed or compressed as it passes from the spinal column between the vertebrae. The injection contains a steroid medication or anesthetic and is administered to the affected part of the nerve.
Epidurals can be diagnostic (an isolated nerve is injected with anesthetic to see if it is the source of pain) or therapeutic (both an anesthetic and an anti-inflammatory medication, such as a steroid (cortisone), are injected near the affected nerve).
Nuclear medicine is often used together with CT, ultrasound and MRI to show how well organs and other structures are functioning. Radiotracers are ingested (swallowed, inhaled, injected, or by eating cookies) to illuminate functions in the bones, heart, brain, liver, bladder or kidneys. Nuclear medicine has a very small radiation exposure and has been performed on children for decades with no known side-effects.
Pelvic venography helps diagnose women whose pelvic pain is caused by swelling of pelvic veins (pelvic congestion syndrome). To treat the condition, the radiologist inserts a thin catheter, about the size of a strand of spaghetti, into the femoral vein in the groin and guides it to the affected vein using X-ray guidance. To seal the faulty, enlarged vein and relieve painful pressure, an interventional radiologist inserts tiny coils often with a sclerosing agent (the same type of material used to treat varicose veins) to close the vein.
Needle electrodes are inserted through the skin and into the site of a tumor in the kidney, liver, prostate or lungs. The radio waves emitted by the probe create heat in the tissue, and the heat kills cancerous cells in a small area around the probe.
If an abscess has formed in the lungs, an interventional radiologist can use images to direct placement of a needle into the affected area for drainage. The drainage tube (catheter) can be guided by CT, fluoroscopy, ultrasound or X-ray.
Magnetic resonance imaging (MRI) of the prostate uses a powerful magnetic field, radio waves and a computer to produce detailed pictures of the structures within a man’s prostate gland. It is primarily used to evaluate the extent of prostate cancer and determine whether it has spread. It also may be used to help diagnose infection, benign prostatic hyperplasia (BPH) or congenital abnormalities.
Treatment for prostate cancer can involve image-guided radiation therapy. In some advanced treatments, daily image guidance is increasingly used to improve the setup due to organ movement. Since the prostate position varies day-to-day depending on bladder and rectal filling, the prostate position must be localized and verified prior to each treatment.
In one method, several fiducial markers, or tiny pieces of biologically inert metal such as gold, are placed in the prostate gland before the simulation. Digital X-ray images are taken which localize the metallic markers to check the position of the prostate on a daily basis just before the treatment, and the prostate is appropriately adjusted and aligned to the planned high-dose radiation treatment field.
Another method involves using ultrasound to localize the prostate before each treatment. The patient is asked to keep his bladder full as much as possible in order to produce a good ultrasound image, and also to displace the bladder mucosa out of the radiation treatment field.
A third method involves the use of a low-dose computed tomography (CT) scan of the prostate area in the treatment couch right before each treatment to verify prostate position. Depending on your case and available technology at your treatment center, your physician will inform you of the type of image-guided radiation therapy you will receive.
Ultrasound is a non-invasive procedure that uses sound waves to image the structure and movement of the body’s internal organs, as well as blood flowing through blood vessels, in real-time. The prostate gland and surrounding tissue are examined by the insertion of an ultrasound probe into the patient’s rectum. There are no harmful effects, and it gives a clearer picture of soft tissues than X-ray images.
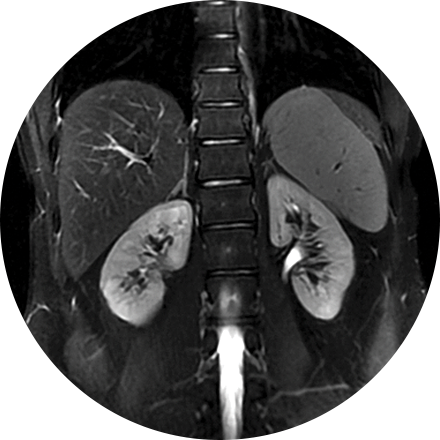
A renogram uses small amounts of radioisotopes to measure the function of the kidneys. This test evaluates the size, position, shape and function of the kidneys. A renal scan is particularly useful when there is a known sensitivity to the contrast media used in an IVP or other X-rays, or when there is underlying kidney insufficiency (reduced kidney function, as after a transplant). A renogram may be used to evaluate kidney function in people with hypertension or to check for rejection after a transplant.
Stents can be used to repair torn aortas, reducing the risks involved in surgical treatments. A stent is inserted into a blood vessel through a small incision in the groin. The radiologist uses imaging techniques to then guide the stent to the injury site.
Stereotactic biopsy uses mammography to precisely guide clinicians to a lump or abnormality such as an area of calcification, that cannot be felt or seen on ultrasound. Clinicians see a 3D picture of the lump’s exact location.
Image-guided biopsy allows patients to avoid hospitalization and general anesthesia (previously necessary with traditional surgical biopsy). It is a valuable method of getting a fast, accurate, conclusive diagnosis—without unnecessary time, pain or expense to the patient.
Transvaginal ultrasound imaging of the abdomen uses sound waves to produce pictures of the structures and organs in and around a woman’s uterus. Transvaginal (TV) ultrasounds are performed very much like a gynecologic exam and involves the insertion of an ultrasound transducer into the vagina to study the lining of the uterus. These exams are frequently used to evaluate the reproductive and urinary systems. Ultrasound is safe, noninvasive and does not use ionizing radiation.
CT or other imaging tools are used to guide the insertion of needles or tubes to drain abscesses.
This specialty focuses on urinary tract and kidney disorders. Renal hypertension puts stress and increased pressure on the kidney and is a major cause of end-stage renal disease. Interventional radiologists can perform angioplasty and, if needed, stenting, to improve blood flow to the kidney. Balloon angioplasty and stenting has generally replaced surgery as the first-line treatment for renal arterial occlusions.
Uterine Fibroid Embolization (UFE) decreases the pain and bleeding of uterine fibroids (benign tumors from the wall of the uterus) by cutting off their blood supply.
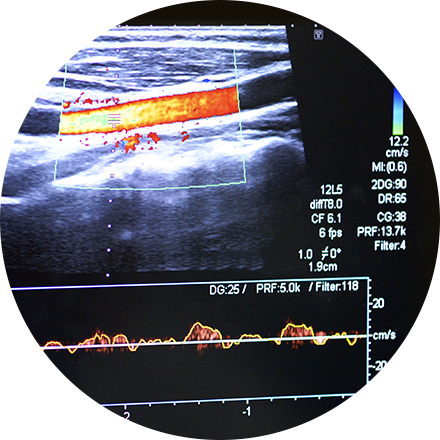
Vascular ultrasound uses sound waves to image the body’s veins and arteries. A special ultrasound technique, called Doppler, evaluates blood flow through vessels in the abdomen, arms, legs, neck and head. It helps the physician find tumors, congenital malformations, narrowing (as with plaque accumulation), and blocks (as with deep-vein thrombosis). It also helps clinicians assess the health of the arteries before or after a procedure, i.e., to judge whether an angioplasty is advisable or if a graft is succeeding.
This is minimally invasive treatment of varicose veins in one or more outpatient procedures.
Vertebroplasty and kyphoplasty are procedures that treat spinal fractures or compressed / collapsed vertebrae, often performed by a neuroradiologist. Vertebroplasty is the injection of a cement-like material into the bone to make it more stable. In kyphoplasty, the doctor first creates space by inflating a balloon-like device in the bone. The space is then filled with the cement material.
Colon cancer risk increases with age, especially for individuals over 50 years old. However it is worthwhile noting that the majority of all colon cancers occur in people who have no risk factors.
Virtual colonoscopy is a relatively new procedure that allows our highly skilled radiologists to recreate and evaluate the inner surface of the colon in a way that has never before been possible. It utilizes a combination of the latest CT technology and sophisticated image processing computers to generate images of the colon from start to finish. When the exam begins a small tube is placed in the rectum to allow for air to be introduced into the colon. You will be requested to hold your breath several times while the the "high speed spiral CT" rapidly scans your abdomen. It is a minimally invasive and painless test and takes approx 15 minutes. You will able to resume normal activity directly after the procedure.
This exam is most commonly used for diagnosing metastatic disease or primary bone cancers. It may also be used to diagnose Paget’s disease, fractures (old vs. new or post trauma), unexplained bone pain, and other bony abnormalitites.
The procedure itself is non-invasive and simple. The patient receives an intravenous injection of a radiotracer. There are virtually no side effects or allergic reactions to this or any other radiopharmaceutical. The patient may leave after injection and return approximately 3 hours later for the scan. You’ll be asked to lie still on a table while an armlike device supporting a tracer-sensitive camera passes back and forth over your body. Patients are encouraged to stay well hydrated to improve the images. Otherwise they may resume their normal routine. The whole body bone scan takes approximately 45 minutes to one hour for most patients.
Because the radiation dose comes from the injection not the camera, additional images may be obtained of any area of interest, sites of pain, etc. without additional exposure for the patient.
A whole body scan can be appropriate for a high-risk patient with a history of heart disease, cancer, smoking, hypertension, or diabetes, or one who has been exposed to hazardous chemicals. The prime benefit of whole body scanning is the ability to locate and diagnose a disease process that can be effectively treated if found early, such as gall stones, degenerative and arthritic changes of the spine, kidney stones, abnormal lymph nodes and many other issues. Logistics are similar to the standard CT discussed on this page.