Case Study – Chronic Noninfectious Osteomyelitis (CNO)
Case Summary
The patient is a 16-year-old male who developed right leg pain after playing basketball while wearing sandals. This was initially thought to be stress related and treated conservatively with rest. The pain was slightly worse at night and responded to Tylenol. The patient was not given aspirin or other NSAIDs due to his history of inflammatory bowel disease, which had been present for many years and under control with the use of low dose methotrexate therapy.
On clinical exam there was point tenderness to the proximal tibia. No sign of redness or abrasions to the skin. There were no systemic symptoms such as fever, chills, or rashes.
The patient had an outside x-ray taken that was reported to be suspicious for a potential sarcoma (figures 1 and 2). An MRI was ordered for further work-up, which after reviewing, was then followed by a CT scan to evaluate for a potential osteoid osteoma nidus.
Imaging Findings
X-ray demonstrated marked wavy solid cortical thickening along the posterior cortex of the tibia (Figures 1 and 2). The periosteal reaction was thought to be non-aggressive in type without evidence of a Codman’s triangle or “onion-skin” appearance.
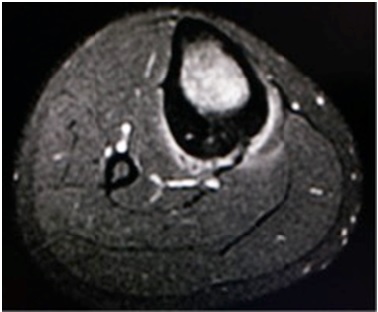
On MRI, there is marrow edema in the thickened posterior cortex with mild adjacent soft tissue edema (figures 3 and 4). Linear vascular grooves are demonstrated in the cortex without radiation to a focal osteoid osteoma nidus.
A CT demonstrated marked cortical thickening with extensive vascular grooves but without radiation to a focal osteoid osteoma nidus (figures 5 and 6).
The differential diagnosis at that time included chronic osteomyelitis, osteoid osteoma with a small nidus not detected on CT, unusual stress/insufficiency fracture possibly related to long term methotrexate use, or less likely sclerosing parosteal osteosarcoma.
A pediatric surgical oncologist was consulted and a needle biopsy was first performed, which was non-diagnostic. An open biopsy was then performed. All cultures and histology were negative for infection or neoplasm. The only abnormality demonstrated was chronic inflammation with lymphocytic infiltrates. The erythrocyte sedimentary rate (ESR) was minimally elevated, however, the white blood cell count remained normal. Next, a nuclear medicine bone scan was performed to evaluate for potential multi-focal osseous lesions and demonstrated only the proximal right tibia to be abnormal in uptake.
FINAL DIAGNOSIS – Chronic nonbacterial Osteomyelitis (CNO)
Discussion
Chronic nonbacterial osteomyelitis (CNO) is a sterile osteitis of unclear etiology. Both single and multiple lesions have been described with a female to male ratio of 2:1 and a mean age of onset around 10 years [1-3]. The most common osseous locations in children and adolescents with CNO involve the metaphysis of the long bones of the lower extremities as well as the pelvis, spine, clavicle, and mandible; however, the osseous lesions can occur at any site.
Non-osseous organs can also be involved with inflammation including the eyes, skin, gastrointestinal tract, and lungs. Chronic recurrent multifocal osteomyelitis (CRMO) is considered the pediatric form of the SAPHO syndrome (synovitis, acne, pustulosis, hyperostosis and osteitis) and is the most severe form of CNO. In one study of seventy patients with CNO, half of the patients had comorbid autoimmune diseases, and 49% had a family history of autoimmunity [3].
CNO is diagnosed by exclusion after ruling out other potential causes such as malignancies such as sclerosing parosteal osteosarcoma or Ewing sarcoma. Benign causes including osteoid osteoma, bacterial osteomyelitis, stress/insufficiency fracture, osteonecrosis, and osteopetrosis are other potential possibilities. Currently, diagnosis is made by the clinical picture, laboratory data, radiological and magnetic resonance imaging (MRI) studies, technetium bone scan, and microbial and histopathologic analysis in a multidisciplinary approach.
Non-steroidal anti-inflammatory drugs (NSAIDs) have been recommended as a first-line therapy and seem to be safe and effective. Disease-modifying anti-rheumatic drugs (DMARDs), steroids, bisphosphonates and TNF blockers have also been used in severe disease manifestations, frequent relapses, and associated inflammatory diseases [3].
Bibliography:
-
Girshick HJ, Raab P, Surbaum, et al. Chronic non-bacterial osteomyelitis in children. Ann Rheum Dis. 2005;64(2):279-285
-
Jansson A, Renner ED, Ramser J, et al. Classification of non-bacterial osteitis; retrospective study of clinical, immunological and genetic aspects in 89 patients. Rheumatology (Oxford). 2007;46(1):154-160
-
Borzutzky A, Stern S, Reiff A, et al. Pediatric chronic nonbacterial osteomyelitis. Pediatrics 2012, 130(5): 1190-1197






Add new comment